A Remote Care Hierarchy
 A lot of my work over the past 6 months has been as part of a team setting up Virtual Wards in Lincolnshire. This has been a collaborative effort across our system featuring input from our community, acute, mental health, primary care and care provider organisations. We’ve been successful in getting the frailty virtual ward up and running with small number (but big impact!) and colleagues have been successful with the cardiology virtual ward (which I can’t take much credit for!).
A lot of my work over the past 6 months has been as part of a team setting up Virtual Wards in Lincolnshire. This has been a collaborative effort across our system featuring input from our community, acute, mental health, primary care and care provider organisations. We’ve been successful in getting the frailty virtual ward up and running with small number (but big impact!) and colleagues have been successful with the cardiology virtual ward (which I can’t take much credit for!).
But if we set up virtual wards in isolation, we’re at risk of people dropping off another edge - if they successfully avoid an admission to hospital or are ‘stepped down’ earlier - what happens then? Does the remote monitoring stop - what if those people had started to take notice of their own observations and were using these to manage their health? There is clearly a need to think about how remote care works across the system.
As part of the work on virtual wards I attended a webinar where this slide was shown
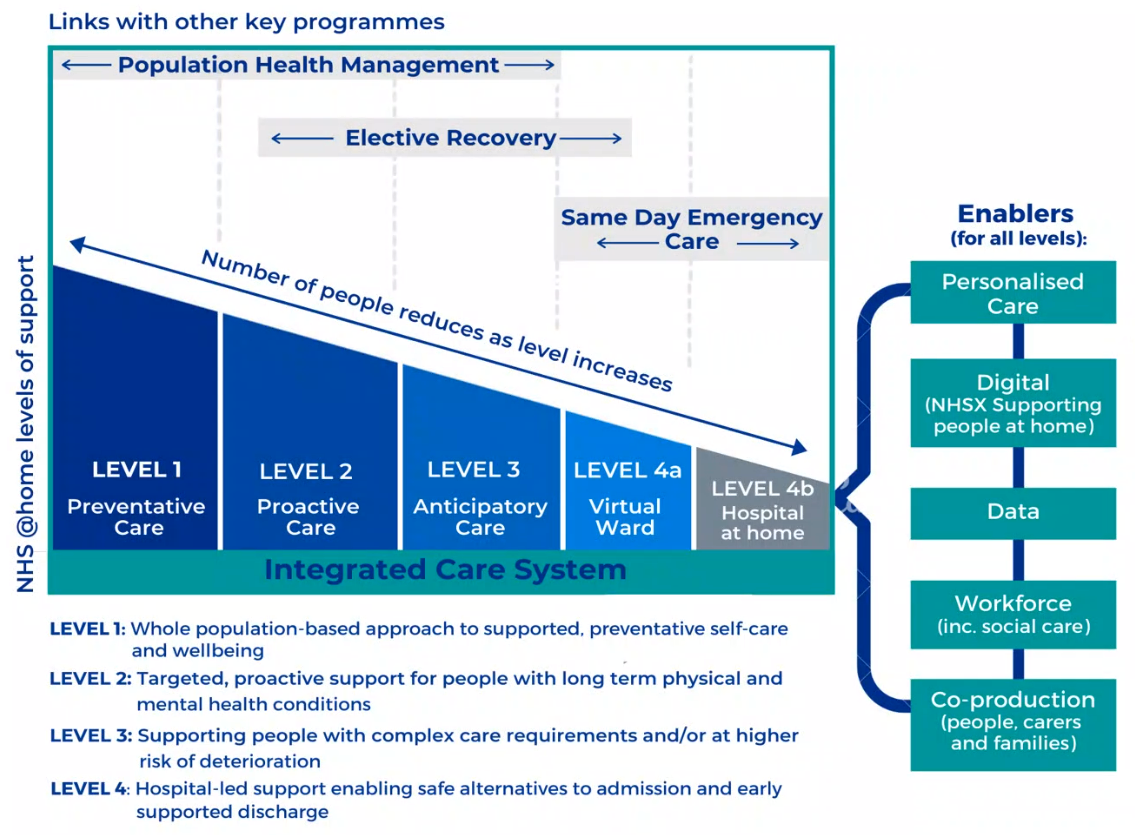 I really like this idea and being shameless, I stole and adapted it to meet the needs for a hierarchy locally.
I really like this idea and being shameless, I stole and adapted it to meet the needs for a hierarchy locally.
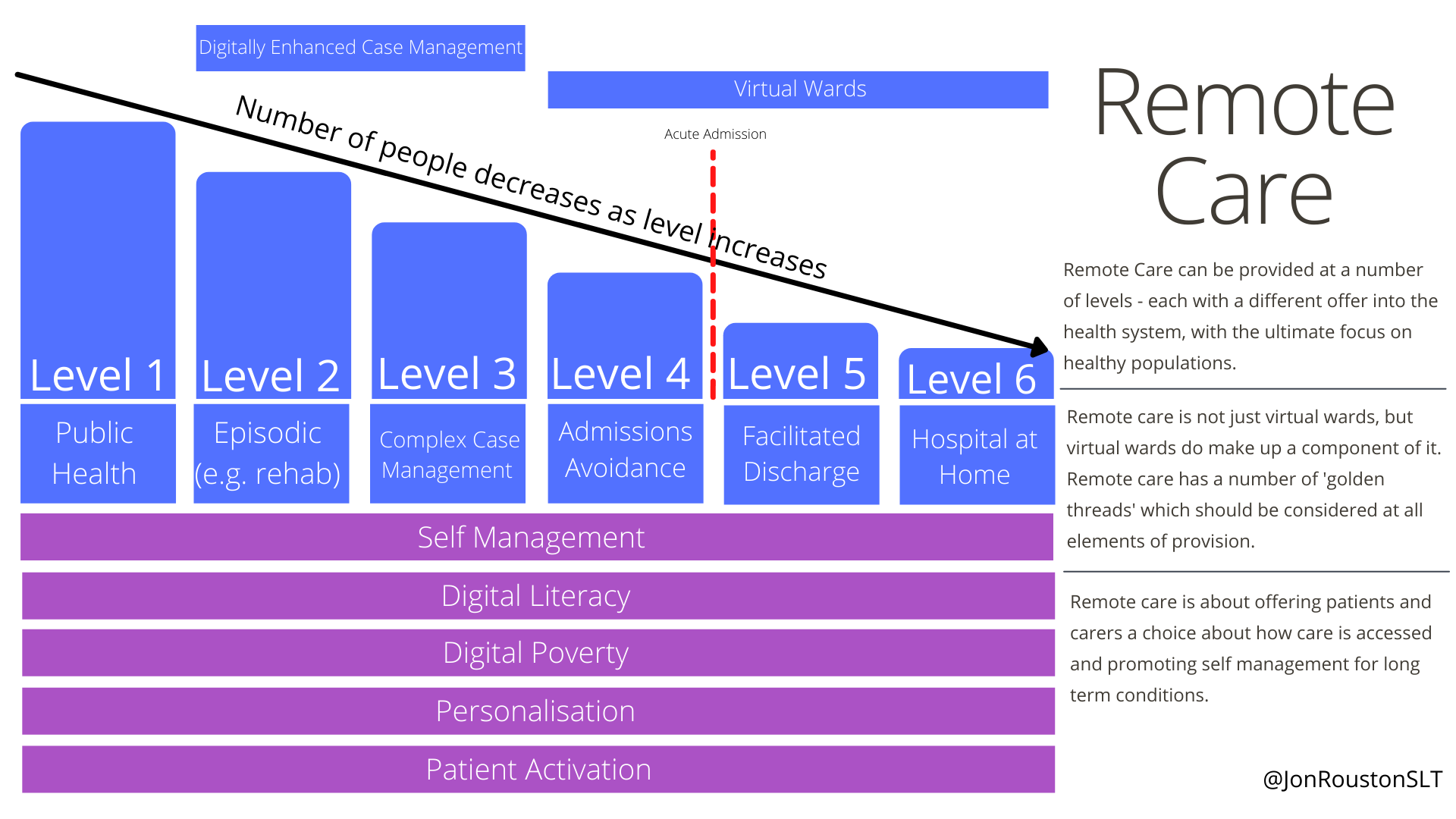
So this is where our thinking is at the moment
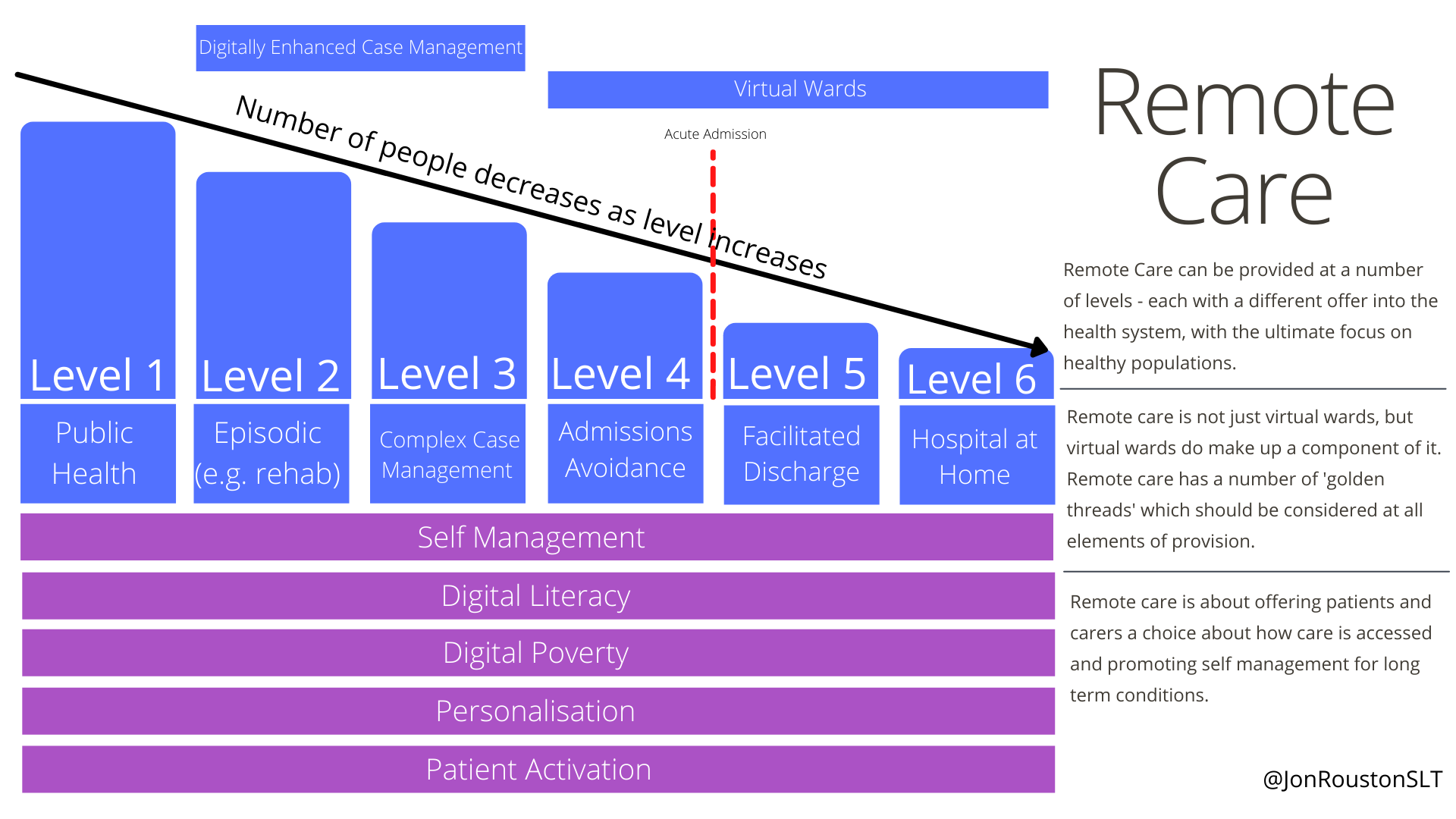
It follows the same model of decreasing population with acuity - but the levels are slightly different as it is looking at how we offer this within our system and how we might support someone across the different phases of their condition.
Level 1 - Public Health
This is information that is freely available to everyone. Our challenge as a trust is to make this as accessible as possible and move towards videos, podcasts and other resources, where previously the humble patient information leaflet may have ruled. This information will help people manage their long term conditions, but is unlikely to be tailored to them. Having said this - we are considering a ‘bank’ of information that can be recommended - so there is tailoring to some degree. The technology underpinning this is likely to be websites and open distribution of resources as above.
Level 2 - Episodic Care
This is short term remote care for people in order to recover from, or sustain an element of their long term health condition. Examples in our trust are cardiac rehabilitation programmes (usually a 6 week programme), pulmonary rehab, stroke rehab and parkinson’s input. These programmes are all of a similar ‘type’ - this is just because the trail was blazed by cardiac rehab and other services that could see similar benefits followed. But there is no reason why this couldn’t be a 2 week educational course etc. The technology underpinning this is likely to be video consultations, group video sessions, monitoring and between session feedback (e.g. reporting episodes of breathlessness over the programme to see if this has improved).
Level 3 - Complex Case Management
This is longer term care for those people with Long Term Conditions (LTC) such as Heart Failure, COPD, Parkinsons etc. This is really where remote monitoring and other technologies come into their own. This gives the clinician more information about the person’s condition and is a tool to enable co-production of health plans with the person who has the LTC. The people at this level are not requiring secondary care at this point and this would be managed alongside Primary Care. Ideally all of the systems we use between primary care and community all talk to each other (are interoperable) so the person interacts with as few systems as possible (does not have to repeat themselves!).
Level 4 - ‘Admissions Avoidance’
I would rather Level 4 and 5 were termed something like ‘care in the most appropriate setting’ but there are terms already out there that better describe what we’re doing and in this case - Level 4 is about Admissions Avoidance. Having someone whose health is declining and is ‘at risk’ of having a preventable admission into hospital - likely through ambulance services, ED etc. This is covered by one half of the virtual ward, which aims to spot people whose health is declining and wrap acute level care around them whilst they remain in the community. In Lincolnshire the form of the virtual ward differs depending on the speciality (I will write about these in a later post) - so how we avoid that admission differs depending on the ward - but the aim is the same. We recognise that this part of remote care has a huge impact on the patient and the care system. Avoiding an unecessary admission is better care for the person, gives better outcomes by reducing them to secondary care risks, costs the system less and reduces demand so that the capacity an be used for those with an unavoidable admission. Key technology for enabling this depends on the ‘ward’ but remote monitoring and the ability to conduct an MDT and appointments via video conferencing (across organisations) have been very important in our system.
Level 5 - ‘Facilitated Discharge’
Otherwise known as ‘Early Assisted Discharge’ - this is simply getting people out of hospital more quickly, reducing the risks of the secondary care environment. The Lincolnshire Frailty Virtual Ward has, anecdotally, managed to discharge frail people 24-48 hours earlier using a EAD virtual ward - for those people who looked to be recovering but the clinician wanted one more days of bloods to check - these people can now go home and these bloods can be done in the community, for the clinician to review and then make a plan jointly with the MDT. Sometimes these people come back in to hospital and that’s OK - we can usually bring them into SDEC for treatment, rather than through ED, which is a better experience for the patients and the clinicians. The MDT working is extremely important for EAD to work and the trust between teams, often across silos needs to be cemented. We can never manage a 100% safe discharge, but there is never a 100% safe admission - life is not 100% safe! Where teams understand the risks and have agreed them jointly - we see much better outcomes.
Level 6 - Hospital at Home
I am going to admit - this one might need taking off the list now as it’s functions might be covered by virtual wards. When conceptualising this I had thought that this might be longer term hospital level care at home for e.g. people at the end of life, but I think this is covered elsewhere in our system. However, for full disclosure - it stays here at the moment - to show this process is iterative!
Golden Threads
As well as each of the levels we also have a number of ‘Golden Threads’ that should run through all of the remote care work. These are:
- Self management - remote care should be used as a facilitator for the wider health aim of people being able to manage their own long term condition. This should be considered at all stages including the virtual wards. How does remote care enable people to self manage their care
- Digital Literacy / Digital Poverty - any remote care programme will need to consider how able people are to access the technology and whether they have access to the devices they need. These could be bannered together as Digital Inclusion
- Personalisation - remote care can be an enabler of delivery of care in a way which is personalised to the individual. It will not happen just because we are using technology - but with the principles of personalisation in mind we can make technology an enabler of that personalisation.
- Patient Activation - Remote care needs to build in methods to identify levels of patient activation and use these to understand how to address the needs of both those who are and are not ‘activated’.
Our job in the forthcoming future is to identify how each of the services we provide can provide care at each of these levels.
I’m very happy for any feedback on this work and would love to see it developed or to see alternatives if you feel there is a better way.
Jon Rouston - @JonRoustonSLT - jonrouston@nhs.net
